
Video otoscopy represents an unsurpassed opportunity to enhance the professional quality of both dispensing and non-dispensing hearing health care practices. This technologically advanced video-optical technique for examination, display and documentation of the external ear canal and tympanic membrane status has become available and affordable in an integrated system (Fig. 1) for routine use in hearing health care practices.

Figure 1. Star-Med integrated video otoscope system (Starkey Labs). Fiber optics light source and accessories for cerumen management are housed in the cabinet.
The narrow diameter of the video otoscope optical probe (2.7mm W x 34 mm L) permits an exceptionally wide viewing angle, allowing a full-field circumferential image of the entire tympanic membrane. Routine use of a 3.0 mm diameter speculum provides a wide berth of maneuverability within the extemal ear canal. This results in a dynamic video display of canal topography and obstructions which cannot be achieved with either a traditional otoscope or with a stereoscopic operating microscope using a hand-held aural speculum. Otoscopic viewing of the pediatric ear canal can be accomplished rapidly with minimum meatal distension, discomfort and head movement interference. Single, multiple or strobed images may be quickly obtained, frozen and inspected after removal of the speculum from the child's ear.
The integrated video otoscope system has the ability to freeze, split and strobe frames. In the split mode, the screen image may be divided into 4, 9, 16 or 25 mini-frames. In the strobe mode, a three second automatic sequence of successive images will be divided into the chosen number of mini-frames. Reproducible documentation is available in an 80-second automated photographic production process with single or multiple copies printed on request. All or a portion of the video otoscopic examination sequence can be recorded on-line via an intrinsic VHS recorder, for example, the effect of a Valsalva maneuver or pneumatic otoscopy on tympanic membrane mobility.
These features of the integrated video otoscope system are invaluable for communication with both physician and patient as well as for continuing clinical self-education. At present, there are at least six generic categories of video otoscopy applications (Table 1).
The video otoscope can be routinely substituted with great clarity and detail for the preliminary standard otoscopic examination which precedes most audiological consultations. When the audiologist or hearing instrument specialist serves as point of patient entry into the hearing health care system, the video otoscope aids in determining the need for patient referral to an appropriate physician resource. Long-term audiological patients can also be monitored and referred for medical consultation based on the symptomatic or asymptomatic outcome of a video otoscopic examination. Abnormalities of the pinna and concha may be optically amplified and recorded. Conditions can be documented which exist within the ear canal and at the tympanic membrane. Middle ear pathology reflected at the tympanic membrane can also be detected.
The video otoscope has numerous unique applications in audiological rehabilitation through custom corrective amplification. A careful assessment of canal suitability for ear impression-taking can be quickly accomplished. Significant accumulations of cerumen can be located and dealt with immediately or through physician referral. Otic pathology which may be contraindicatory to hearing aid use can be identified with photographic documentation available for appropriate medical referral.
An oto-block placement site can be preselected and verified. Having the patient open and close the jaw and smile or grimace broadly while the otoscope is laterally placed within the canal will provide prognostic information concerning temporomandibular joint (TMJ) (Ref. 5) and facial muscle movement effects on custom hearing instrument stability, slit leak and feedback development. By moving the video otoscope within the external canal, an excellent multidimensional clinical impression may be constructed of the geometry of both the lateral cartilaginous and medial bony portions of the canal.
This allows the clinician to identify and mark on the ear impression the optimum positions for receiver tubes and medial vent orifices. Canal anomalies can be verified and either noted for the laboratory on the impression or detailed on the impression in advance. In cases of surgically altered ears, including fenestration and radical mastoid, a safe and effective strategy for single or multiple cotton block placement can be planned and implemented.
At time of fitting, the video otoscope can be effectively used as an adjunct to custom hearing aid orientation. The correct in situ hearing instrument orientation in the ear can be demonstrated on camera. Gain control, microphone, vent and battery compartment can be identified in a full color video close-up. Techniques for proper hearing instrument insertion, removal and gain control adjustment can be modeled in the patient's ear while the patient observes the monitor. By separating the fiber optic light cable from the otoscope head and using it as a spotlight, the cosmetic appearance of the hearing instrument can be shown from frontal, fronto-lateral and lateral points of view. For service and corrective amplification diagnostic information, the video otoscope can be used to identify sebum, desquamation, cerumen and debris in both microphone and receiver ports and in vents. Points of pressure, discomfort and irritation associated with hearing instrument use can be located in the ear, using the video otoscope to relate physical fitting complaints to external ear morphology.
The degree of cerumen interference with various audiological procedures changes with its quantity, texture, degree of impaction and position within the canal. Moving the video otoscope within the canal provides dynamic information concerning each of these variables. Video otoscopy facilitates selection of a treatment strategy selection for cerumenous obstructions of the ear canal.
Direct cerumen management has been identified as within the scope of practice of audiology by the American Speech-Language-Hearing Association. (Ref. 2) The Academy of Dispensing Audiology has sponsored cerumen management seminars.(Ref. 1) The American Academy of Audiology has published a "how-to" article on cerumen management.(Ref. 6) Cerumen may be removed by irrigation, suction, wax removal implements or a combination of the three. Video otoscopy can help the clinician determine the most appropriate strategy for cerumen removal, including the need for ENT referral. Video otoscopic monitoring of cerumen removal during irrigation is neither safe nor practical. However, cerumenous status of the ear can be verified pre- and post-irrigation. The video otoscope may be used, with or without speculum, to monitor cerumen extraction concurrently with the use of suction or appropriate instruments such as wax loops, picks, snares and miniature alligator forceps.
Where cerumen presents for removal by mechanical means, wax loop accessories can be attached directly to the otoscope head (Fig. 2). One version, of the author's design, is mounted on a 3 mm speculum tip in a position approximately 5-8 mm medial to its termination. The other is mounted without speculum directly on the fiber optical shaft.
Figure 2: Two different cerumen removal loops mounted on video otoscope heads. Above: Sullivan speculum loop. Below: Starkey probe loop.
Use of either instrument results in a sharp video image framed within the inner circumference of the 3 mm diameter vinyl wax loop. Because of its fixed orientation, relative to the camera, the image of the loop does not appear to change on the screen. However, the physical location of the loop within the car canal can be manipulated with exceptional accuracy (Fig. 3). As all movements are magnified on the video monitor screen, dexterity in cerumen extraction is quickly refined.
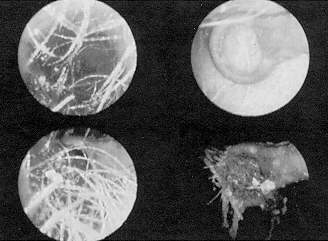
Figure 3. Cerumen removal sequence with Sullivan speculum loop for the video otoscope. Top left: Cerumen in situ; top right: angulated loop entering ear canal; lower left: loop positioned medial to site of cerumen; lower right: cerumen extracted.
Allowing the patient and accompanying party to view the procedure on the video monitor tends to reduce the anxiety which often accompanies the cerumen removal process. The outcome is subject to immediate video-verification. Initial patient stress is considerably relieved in subsequent visits requiring direct cerumen management.
For those practitioners who do not routinely remove cerumen, the video otoscope provides an excellent technique for demonstrating the audiological significance of the cerumen to the patient, and the need for referral to an agreed upon primary care physician (PCP) or ENT physician resource.
Photographic documentation can be provided to the referred physician with a notation of the cerumen's audiological impact. Physicians, both ENT and PCP, occasionally will tell referred patients that "there wasn't much (wax) there." Considering the time and expense involved, this may have a negative impact on the patient's confidence rating in his or her hearing health care provider.
Video verification of cerumen presence to the patient with an explanation of its significance and photographic documentation to the referred physician typically enhances the patient-dispenser, patient-physician and physician-dispenser relationships.
PCP referrals constitute a significant, growing proportion of patients referred to the audiological practice.(Ref. 7) Consistent, repeated evidence of the ability to identify, document and refer treatable otic pathology enhances the audiologist's professional credibility with this physician population. Anomalies and pathology can be photographed, documenting the need for the referral.
For example, in children, blocked or dislodged pneumatic equalization tubes and acute middle ear pathology can be documented and an appropriate pediatrician or ENT physician referral made. Both recognized and undiagnosed pathology and anomalies of the external ear and tympanic membrane can be photographically represented to the PCP, along with the audiological evaluation report.
Parents of pediatric patients are appreciative of the identification, counseling and referral for such conditions as serous otitis, occluded PE tube status, acute purulent otitis, retraction, perforations, et al. With the adult population, the existence of such conditions as abrasions and contusions in the ear canal and perforations and scars of the tympanic membrane can be identified for the patient prior to tympanometry / acoustic reflexes, ear impressions, probe tube real ear measurement, bithermal water or air caloric stimulation and cerumen removal.
When direct visual evidence of the smallest significant amount of cerumen is presented to a patient, the level of motivation is significantly elevated to follow a recommended direct or referred course of management. In the latter case, video otoscopic photo reproduction can be provided to the patient for hand delivery, with referral letter, to the physician.
Obvious patient benefit is realized from in situ visually reinforced instruction in hearing instrument insertion, operation and removal. The patient can actually visualize gain control adjustment, etc. Frontal and lateral images of the custom hearing instrument and the effects of and facial muscle movement can be shown in situ. The need for hearing instrument service due to obstructed transducers can be shown. Patients consistently comment favorably on the highly apparent technological level of hearing health care practice where video otoscopy is used.
When using video otoscopy on a regular basis, the hearing health care practitioner develops an intimate awareness of the variations of normal and pathological anatomy in the external ear and at the tympanic membrane. Two excellent color reference texts are available (Refs. 3,4) with illustrations of ear canal and tympanic membrane pathology presenting a field of view similar to the video otoscope. Conductive overlays and impedance findings can be visually correlated with tympanic membrane appearance.
Derived morphological information and counseling support lead to improved hearing instrument fitting skills. Direct cerumen management techniques are improved by constant video self-reinforcement, especially when the cerumen loop is mounted directly on the video otoscope probe or speculum.
The practitioner's patient rapport and professional image are enhanced by having video otoscopy as a patient counseling tool. The practitioner's professional level of communication with PCP and ENT physicians is elevated, as well. This invariably facilitates future professional physician interaction with the potential for increased referrals. Other video otoscopy applications will arise as use becomes more widespread.