Wow! That's cool!. A chronology of some of my most vivid memories: 1969 - very pleased with my uniform Bekesy tracings; 1971 - discover that my tympanograms are rather wimpy; 1974 - relieved to see my ABR Wave V at 5.76; 1981 - amazed that my REUR is so similar to the KEMAR; 1992 - through the use of video otoscopy, learn that I have an ugly black hair in my right ear canal! We all remember the "wows", "neats", and "cools" when we were first able to view each other's ear canals and tympanic membranes on a video monitor (and even take a photo home with us). Now that the novelty has worn off, we're beginning to sort out the true practical applications of this technology. Once considered little more than an expensive toy, in a few short years, video otoscopy has become a routine clinical tool for many practitioners.
In this month's Page Ten "Hands On" article, we're fortunate to have one of the pioneering video otoscopy people, Roy F. Sullivan, Ph.D.
Roy has a private practice, Sullivan and Sullivan, in Garden City, NY and, as many of you know, he is well recognized for his informative workshops and seminars. Dr. Sullivan, never one to shy away from new techniques, was one of the first audiologists to routinely use video otoscopy in his private practice. This month on Page Ten, he provides us with an excellent summary of the may applications of this procedure. For you high-tech types, the next time you're "surfing the web", check out Roy's Video otoscopy Forum with 24-bit color illustrative case studies. Cool.
Gus Mueller Editor,Page Ten
In the three years since the introduction of video otoscopy [VO] to the hearing health professions by Starkey-JedMed(Ref. 1) more than one thousand systems have been purchased and placed into routine clinical operation by audiologists and hearing instrument specialists. Today,VO instrumentation is available in both clinical and portable models from a number of manufacturers including Grason-Stadler (Welch-Allyn), Siemens, MedRx, Rexton and Starkey (JedMed). MedRx supplies VO units for Argosy, Beltone, Electone, Finetone, Hal-Hen, HSI, Lori Labs, Magnatone, Maico, Miracle Ear, Micro-Tech and Qualitone. A number of companies, including Lori Labs and Starkey/Pro-Hear, have computer interfaces for VO(Ref. 1)
Video otoscopy is an invaluable clinical tool for the hearing health professional. To apply it beyond the "Gee whiz, look at that earwax!" stage, the practitioner may require continuing education to acquire or reacquire a familiarity with the normal anatomical variations and pathology of the outer ear, middle ear and tympanic membrane. Furthermore, there is an established, medically-based vocabulary routinely used by physicians. If you wishes to communicate effectively with the primary-and specialty-care medical community, you must use their language. Medical dictionaries and otology textbooks are good beginning references.
The clinical skill to identify, document and refer otic pathology is essential for those professionals who wish to enjoy a broad referral base among primary-care physicians [PCPs]. The PAGE 10 "hands-on" format lends itself to a sampling of the multiplicity of VO uses which soon become apparent in routine clinical practice. A summary table of VO applications (Appendix Table 1) is found in the Appendix.
Each of the VO images included in this article was selected from cases seen in my own audiological practice which is limited to the fitting of hearing instruments in adult patients, largely referred by PCPs. Figures were either captured directly to computer storage using a Starkey/Starbase VO system or were scanned into computer memory from prior video printer photographs.
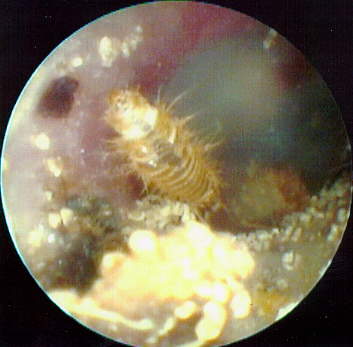
There are conditions of the external auditory canal [EAC] and of the middle ear, manifest at the tympanic membrane [TM], which may influence acoustic and physical access for audiological diagnostic and hearing aid-related procedures.They can be categorized as canal anomalies, endogenous residue, exogenous factors, external otic pathology, TM perforations and status post -ME surgery. [For browsers with html 3.0 TABLES capability, view Appendix Table 2 from this link. Use the BACK arrow to return here]
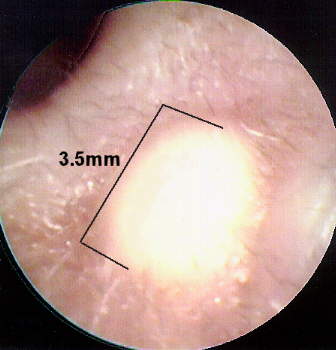
Figure 1 illustrates how an otherwise insignificant amount of cerumen can impact on a real-ear-probe-microphone tube measurement.

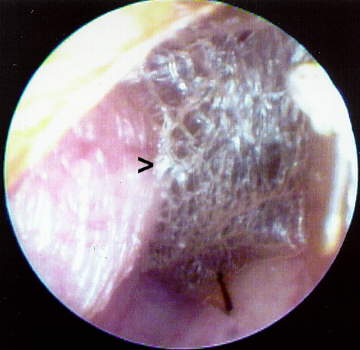
Figure 2 shows the presence of a desquamation web or neomembrane totally occluding the EAC. The audiometric profile for this case revealed a mild (10 dB - 15 dB) conductive overlay with a normal (type Ad) tympanogram. The condition had been previously misinterpreted elsewhere as a scarred TM. Removal of the web, by an otolaryngologist [ENT], resulted in a closure of the air-bone gap.
In many instances, I have been able to use VO to help explain my audiological findings. For example, in one interesting case (Figure 3), I observed an atelectatic TM virtually "shrink wrapping" the ossicular chain. This observation concurred with my test results showing a 35-50 dB air-bone gap and a flat tympanogram.

Miniscule perforations can be differentiated from monomeric scars by placing the endoscopic lens deep within the EAC , thereby allowing a full view of the TM, including the annulus and vascular strip. It is possible to verify the presence of a monomeric TM scar with use of the VO intrinsic Siegle/Politzer bulb and then correlate that observation with an abnomally peaked (Type AD) tympanogram. The presence of an occluded TM perforation can account for an abnormally elevated equivalent EAC volume [PVT]. Observable TM scarring can suggest causation of absent acoustic reflexes.
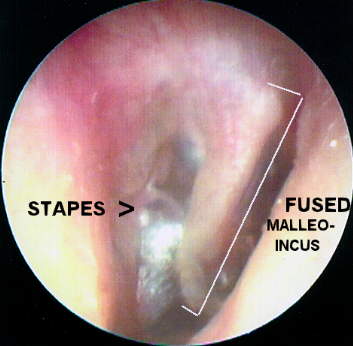
Figure 4 presents a congenitally fused, hypertrophic malleo-incudal complex resulting in an 65 dB conductive overlay. The condition was ruled inoperable during exploratory tympanotomy because of facial nerve anomalies within the middle ear space.
With increasing frequency, the audiologist serves as point of entry for patients into the hearing healthcare system, either through direct acquisition or upon referral from a PCP. Consequently, both audiologists and hearing instrument specialists are situated at a critical point on the chain of patient care, and bear a clinical responsibility well beyond identifying the so-called "FDA warning signs". VO is an invaluable tool in the hands of a knowledgeable clinician.
Figure 5 represents the left ear of a long-term patient seen for a periodic hearing aid follow-up evaluation after a two year interval. The ear had an unsuccessful stapedectomy 30 years ago. The incudal head of the wire prosthesis has recently begun to extrude through an anterior monomeric scar in the TM. On referral, the consulting ENT recommended monitoring but specified no course of treatment.
Photographic examples of pathology that might be encountered in routine hearing health practice have been presented in the June, 1995 Hearing Journal (Ref. 2). In such cases, VO images are usually consistent with pure tone audiometry and tympanometric findings.
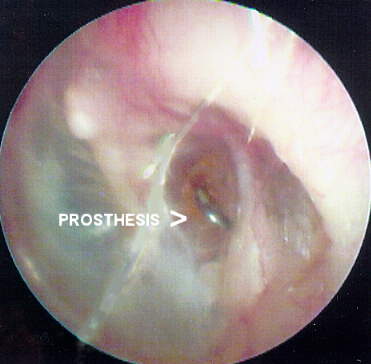
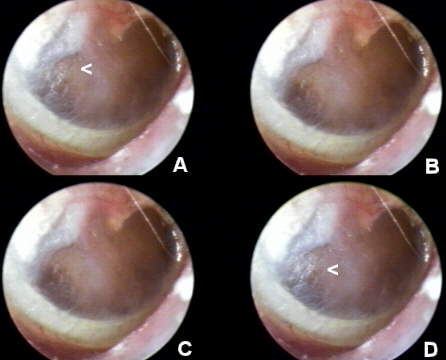
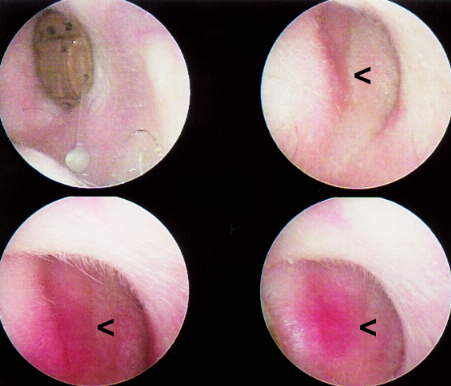
Figure 6 demonstrates the VO strobe feature, which permits a time-based series of images can be sequenced automatically in a "golf swing" analysis. It is useful in viewing the effects of a Valsalva or Toynbee manuever at the TM. In this particular case, the 75 year old female patient was referred by a PCP with chief complaints of chronic hearing loss and an intractible "clicking" tinnitus on the right ear (AD). While the pure tone audiogram revealed a 45 dB, sloping, mixed, essentially sensorineural loss of hearing with an unremarkable (Type A) tympanogram, VO provided a probable etiology for the tinnitus. Examination of the TM at close range revealed an absent manubrium mallei and, posteriorly, a long process of a displaced incus which, because of an hyperpatulous eustachian tube, would intermittently make contact with the TM, functionally coinciding with the "click". Two ENT physicians and an MRI ruled out cholesteatoma an alternative diagnosis. The VO strobe sequence shows the effect of a single nasal respiratory cycle (A-D) on the TM. The patient had unconsciously developed a compensatory mouth-breathing strategy. The intermittent contact can be seen in the area of a posterior, inferior monomeric scar. A (1 mm) vented canal aid was prescribed for the affected ear, providing both hearing help and environmental masking of tinnitus.
VO is important for identifying and demonstrating conditions that require medical attention. It is also of value in establishing a dialogue with physicians on VO observations of clinical interest, especially when related to audiological findings and hearing instrument recommendations. The effect of medical treatment can also be documented, for example, resolution of acute conditions such as otitis externa and otits media.
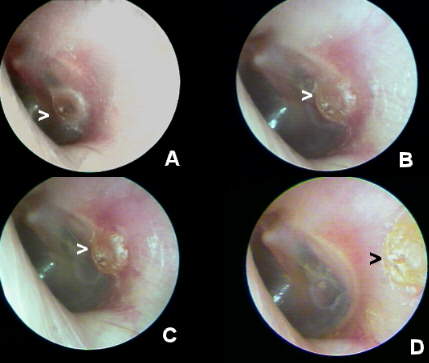
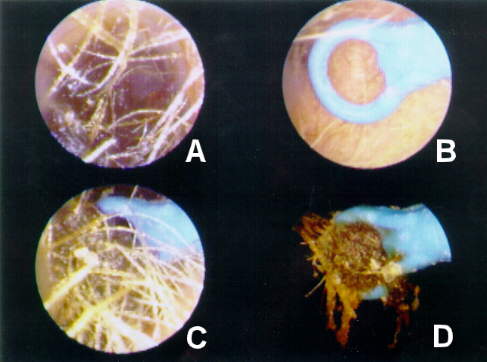
Figures 7a-d shows a sequence of VO records documenting the impact of an ENT-performed office myringotomy of the TM for an acute serous otitis media [SOM] in 70 year old pediatrician. To promote TM healing, the ENT applied phenol to the edges of the paracentesis in order to promote healing and closure. Figure 7A shows the resulting cicatrice as it appeared within 48 hours of the procedure. Note, in Figures 7B-D,the antero-lateral movement of the phenolized TM epithelial layer cicatrice with the normal lateral squamous epithelial migration. The presence of a residual circular keratinization of the medial TM layer at the initial site of incision can be observed, over the sequence, to be non-migratory. The (physician) patient, ENT and PCP were all duly impressed and grateful to be apprised of the clinical case status with this level of clinical documentation. The patient was successfully fitted with a completely-in-canal (CIC) hearing instrument in the noninvolved ear.
rather than inundating the physician with gratuitous, undocumented photographs of the EAC and TM. The audiologist must learn to identify and use the proper medical terminology describing, not necessarily diagnosing, the condition(s) noted in VO. This includes not only pathology of the middle ear manifest at the TM but also epidermal pathology of the EAC , concha and pinna.
VO is helpful in verifying conditions in the external and middle ear that may influence ear selection for monaural fittings. Video otoscopy can be used to range throughout the length of the EAC, determining the presence of cerumen, desquamation or abnormalities that may affect the impression-taking process and that may suggest the relative appropriateness or inappropriateness of a specific hearing instrument morphology. For example, Figure 8 illustrates a set of exostoses which severely compromises the insertion depth for a potential CIC hearing instrument fitting.

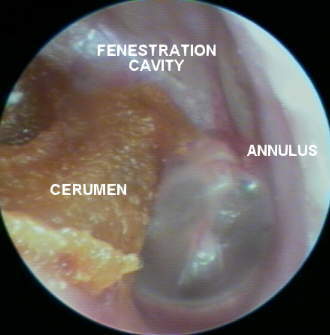
Figure 9 presents the full breadth of a fenestration cavity defining the limits of special care needed in hand-tied otoblock placement for the impression-taking process. [Follow this link for a VO case presentation on impression-taking in cavitated canals. Use the BACK arrow to return here.]
Imperfections and voids in the impression may be filled, based on a VO survey of the EAC landmarks. Impression artifacts can be differentiated from EAC anomalies. Figure 10 shows a benign keratoma at the concha-meatal junction which, unless marked for the shell technician, would invariably be identified as a void in the impression and filled in the shell-making process. The boundary area between cartilaginous and bony canal can be closely explored and ear impressions appropriately detailed in advance of ordering.
In my practice, I use a quick-release wide angle lens attachment for the VO to counsel new hearing aid users on proper methods of inserting, removing and operating the hearing instrument. This is especially helpful with CIC fittings because these instruments present few tactile or visual orientation landmarks easily perceptible to the older population, (including this author).
VO can be employed as a very costly, but highly effective, mirror substitute to show the hearing instrument's cosmetic impact or lack thereof. On more than one occasion, I have used VO to present a vivid display of impacted cerumen in a minicanal aid receiver tube which immediately quelled a patient's tirade about poor hearing instrument quality.
Figure 11 displays a sequence of vignettes demonstrating a CIC-induced contact dermatitis at the anterior concha-meatal junction. Based on this observation, the problem was solved by instructing the laboratory to recast and replate the instrument at a forward 60o angle. I routinely use VO as a guide in identifying and correcting the source of pain and physical discomfort problems in hearing instrument fittings.
Hearing health professionals have become involved in the removal of cerumen, incidental to the requirements of hearing testing or hearing instrument fitting. Table 3 (Appendix) introduces a proposed classification of cerumen accumulation based on audiological access requirements. By observation and probe, VO provides information concerning the most appropriate mode of cerumen extraction, e.g. curettage, lavage, suction, VO-curettage, pre-softening with a wetting agent or a combination of these techniques. In contemporary audiological practice there are two basic formats for cerumen management , referred and direct.
Here is a seven-step program for referred cerumen management:
Here is a procedure for direct cerumen management:
Patients will invariably follow a recommended course of action, be it medical or hearing instrument - related, if you provide them with a visible, comprehensible reason for the recommendation. This applies whether you are referring them to a dermatologist because of an epithelial lesion of the pinna, concha or canal or to an ENT physician because of otic pathology.
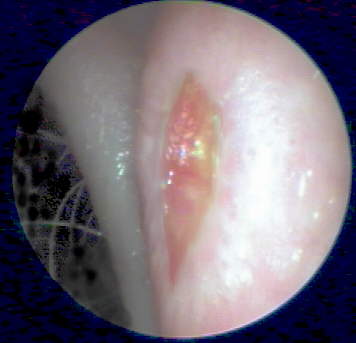
In one case, (Figure 13) an ulceration observed on the posterior anti-helix of an ITE-aided ear during a follow-up visit led an initially reluctant patient to accept my referral to a dermatologist. The lesion was biopsied resulting in a diagnosis of chondrodermatitis nodularis helicis, a painful but benign and medically treatable condition.
Parents of pediatric patients appreciate viewing their child's PE tubes in situ(Ref. 2) to see that an otitis media, which they had viewed in the acute stage, has been resolved with medical treatment. The use of VO for counseling hearing instrument patients has been discussed, above.
Effective application of VO in a hearing care office promotes the perception, by both patient and physician, of technological awareness and clinical astuteness. Having introduced VO into my practice, I received unprecedented complimentary letters from physicians, both ENTs and PCPs. VO coincidentally facilitates a high level of professional marketing.
Once implemented, video otoscopy virtually challenges hearing health clinicians to learn more about the images with which they are confronted. In my practice, I examine an average of fifty ears per day with VO. I save case illustrations of interest or clinical import by computer image capture (Ref. 3) and annotation. I use a Polaroid video printer or high resolution color computer ink-jet printer to reprint images for records and physician reports. E-mail transmission of color images is also feasible. As I stated at the beginning of this article, use of accurate medical descriptors of visible otic symptomatology is essential for the hearing professional's credibility with referring physicians.
By means of self-study, organized continuing education and colloquy with physican colleagues, the clinician can learn to differentiate otic pathology from normal anatomical variations and to identify and describe pathology at the TM as well as dermatological pathology of the outer ear. Hearing instrument morphology selection and modifications skills and cerumen management techniques will improve with VO monitoring.The American Academy of Audiology has co-sponsored 4-hour convention courses on VO (Ref. 4). Several books on otoscopy are listed in the bibliography. (Refs. 5-8) The higher image resolution of direct otoscopic color 35mm photography in these publications is excellent for instructional purposes. (Ref. 4) It can be anticipated that instrument manufacturers and clinical training institutions will sponsor regional continuing education seminars on VO and otic pathology for the non-physician hearing health community.
I have developed a VIDEO OTOSCOPY FORUM for hearing health professionals on the Internet World Wide Web, including 24 bit color VO case studies. Anecdotal information, pure tone audiometry and tympanometry are incorporated, as appropriate. Illustrations from this article are included for enlarged observation or downloading.
For those with the capacity to "surf the web" and view 16 or 24 bit color images, web browser software may be directed to:
Questions about VO may be E-Mailed to:
I. General examination of the ear canal and TM
II. Physician communication
III. Hearing instrument selection and fitting applications
IV. Cerumen management
V. Patient education
VI. Professional image enhancement
VII. Knowledge base / Skill growth
[Select this link for VO examples in each category. Use the BACK arrow to return here]